Cataract Surgery and Glaucoma: How to Handle them Both
Cataracts and glaucoma are common eye conditions that become more prevalent with age. They are different but influence one another in several ways.
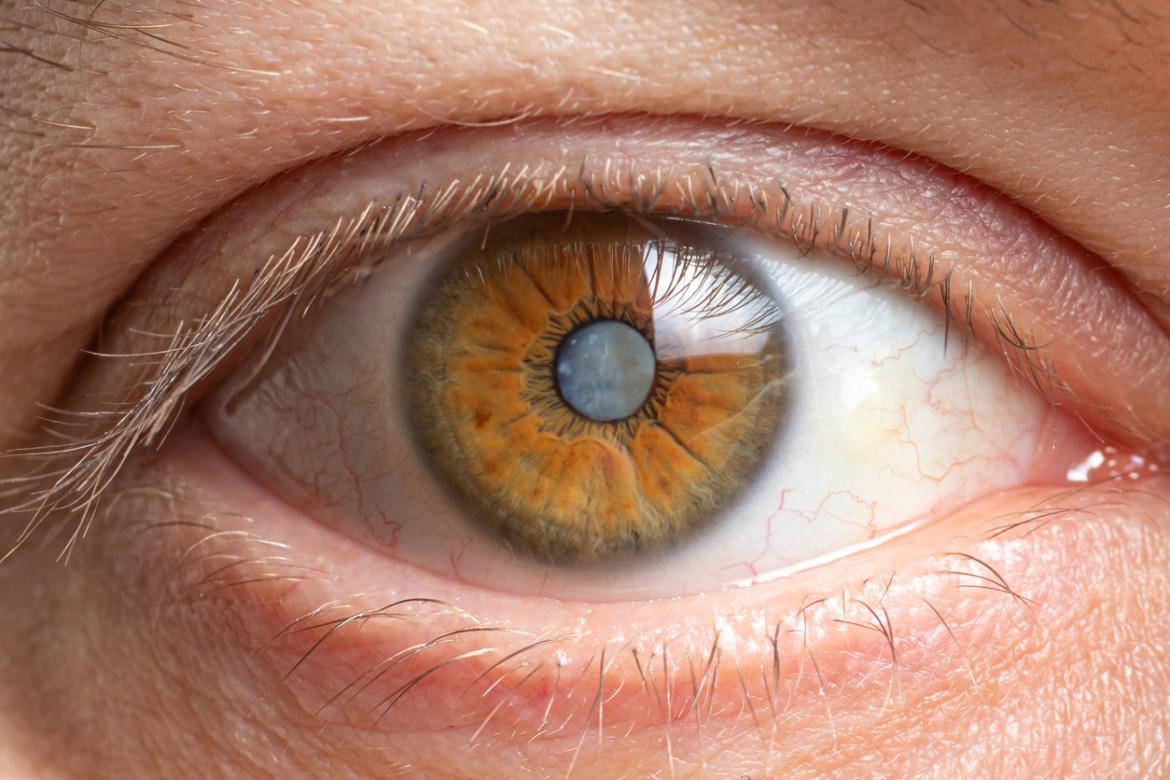
A cataract occurs when the natural lens inside the eye becomes cloudy, obscuring the clarity of vision. Our eyes have a natural lens which focuses light onto our retina. When we are born it is crystal clear, but as we age it slowly acquires opacity. Cataracts cause a reduction in the quality of vision, and reduced color appreciation. They can cause glare, especially at dusk or with oncoming headlights when driving. They can make reading difficult, especially at night when increased lighting is needed. Eventually they become sufficiently bothersome to require cataract surgery. In cataract surgery, the cataract is removed from its bag and a clear, artificial intraocular lens is inserted in its place.
Glaucoma occurs when pressure in the eye damages the nerve that connects the eye to the brain, the optic nerve. Without this nerve we cannot see. In glaucoma, the optic nerve is damaged slowly, but cumulatively; since the process is painless, and tends to affect our peripheral vision first (which we are generally unaware of), we may not notice glaucoma until it is advanced. Once damage occurs it cannot be reversed; but treatment (generally involving lowering eye pressure) can prevent or halt the damage from worsening. That is why it is always best to detect glaucoma as early as possible. Glaucoma is a lifelong condition that requires lifelong monitoring and treatment. It is generally treated by lowering the eye pressure with gentle, safe laser; regular eye drops; or in some cases glaucoma surgery.
As an Ophthalmologist sub-specializing in cataracts and glaucoma, I am often referred patients with both conditions simultaneously. For instance, someone might have visually significant cataracts, and optic nerve features suspicious of glaucoma. Or, someone might have the very beginnings of cataracts, but raised pressure and clear signs of untreated glaucoma. What is the best approach to managing the combination of cataracts and glaucoma?
As I explain to my patients, it is always important to stabilize glaucoma before considering cataract surgery. Cataracts cause reversible loss of vision and hence the surgery can usually be safely deferred; for glaucoma, while true emergencies are rare, there is a degree of time pressure in the sense that every day of raised eye pressure can lead to further optic nerve damage that is irreversible. It is preferrable to have glaucoma addressed first by lowering eye pressure (with gentle laser or drops) before considering cataract surgery, which can often be safely deferred until the timing is right for the patient.
For people with glaucoma and cataracts, I am an advocate for minimally invasive glaucoma surgery devices at the time of cataract surgery; these are microstents inserted into the eye’s drainage pathway, that provide eye pressure lowering. These often allow patients to cease some of their glaucoma eye drops; an important outcome given eye drops all have side effects and cause discomfort and dryness in and around the eyes. Minimally invasive glaucoma microstents are used for patients with mild or moderate glaucoma when they are undergoing cataract surgery.
Rarely a patient with more severe glaucoma needs a formal glaucoma operation (e.g., a trabeculectomy) to stabilize the pressure. A trabeculectomy involves creating a drainage pathway from inside to outside of the eye, allowing fluid to collect safely in a reservoir under the eye’s lining and hidden by the upper eyelid. This can be combined with cataract surgery; but in general, separating the procedures (performing the trabeculectomy first and cataract surgery later) results in safest and best outcomes.
When it comes to managing both cataracts and glaucoma, a tailored approach is important – there are several treatment options and the right choice depend on a variety of factors: the severity of the cataracts, the degree of glaucoma, and the patient’s lifestyle and wishes. A frank and open conversation detailing our approach from the outset, with patients well informed of their options, leads to best outcomes.